Exercise & Nutrition Checklist
Welcome to the
Women’s Wellness Hub
Unlock your potential
Nutrition tips that are not overwhelming
Unlock the potential by just making some small adjustments in your nutritional choices to better support your body through perimenopause and menopause - to increase your energy levels, improve sleep, reduce inflammation, continue to build muscle, reduce hunger pangs and get the right vitamins.
It is not all about weight loss, BMI etc but it about getting the right balance to help us get our groove on and enjoy this chapter rather than get stuck into the vault of negativity due to some weight gain.
Staying hydrated - it makes a big difference!
Realistic exercise tips
Not aiming for a marathon? Nor are we! Body aching? Let's help
Your Paragraph text goes Lorem ipsum dolor sit amet, consectetur adipisicing elit. Autem dolore, alias, numquam enim ab voluptate id quam harum ducimus cupiditate similique quisquam et deserunt, recusandae. here
Get the checklists and tips you need to keep
on top of key women's physical health issues
PREPARING TO SEE YOUR GP
Often we make appointments with our GP only because we feel there is something wrong with us - in turn we often only get 'reactive care'.
We often walk in knowing we have symptoms or have just not been 'for ages' and go in relatively ill-prepared.
Many of us then unrealistically expect that all our health issues can be reviewed and considered in the average 10- 15 minute GP consultation. This is usually only enough time dedicated to briefly talking about 1-2 relatively minor health issues you may be experiencing. If you need a thorough health review, or a longer appointment to talk about your symptoms, then you mightneed a longer appointment (you can often ring the clinic or go onto their website to book a longer appointment). Fees will vary depending on the time you book, whether they bulk bill, you have a medicare card etc.
Some clinics offer telehealth.
We avoid the 'proactive' care and checkups blaming being time poor, not knowing what to ask for or feeling uncomfortable about the appointment, but the reality is the proactive is often more critical. You can avoid huge wellness, financial, employment, relationship and mental health issues if you are proactive in your care and get educated and know what to ask for and when.
Regular health check-ups can identify any early signs of health issues. Finding problems early means that your chances for effective treatment are increased. Many factors, such as your age, health, family history and lifestyle choices, impact on how often you need check-ups.
IMPORTANT:
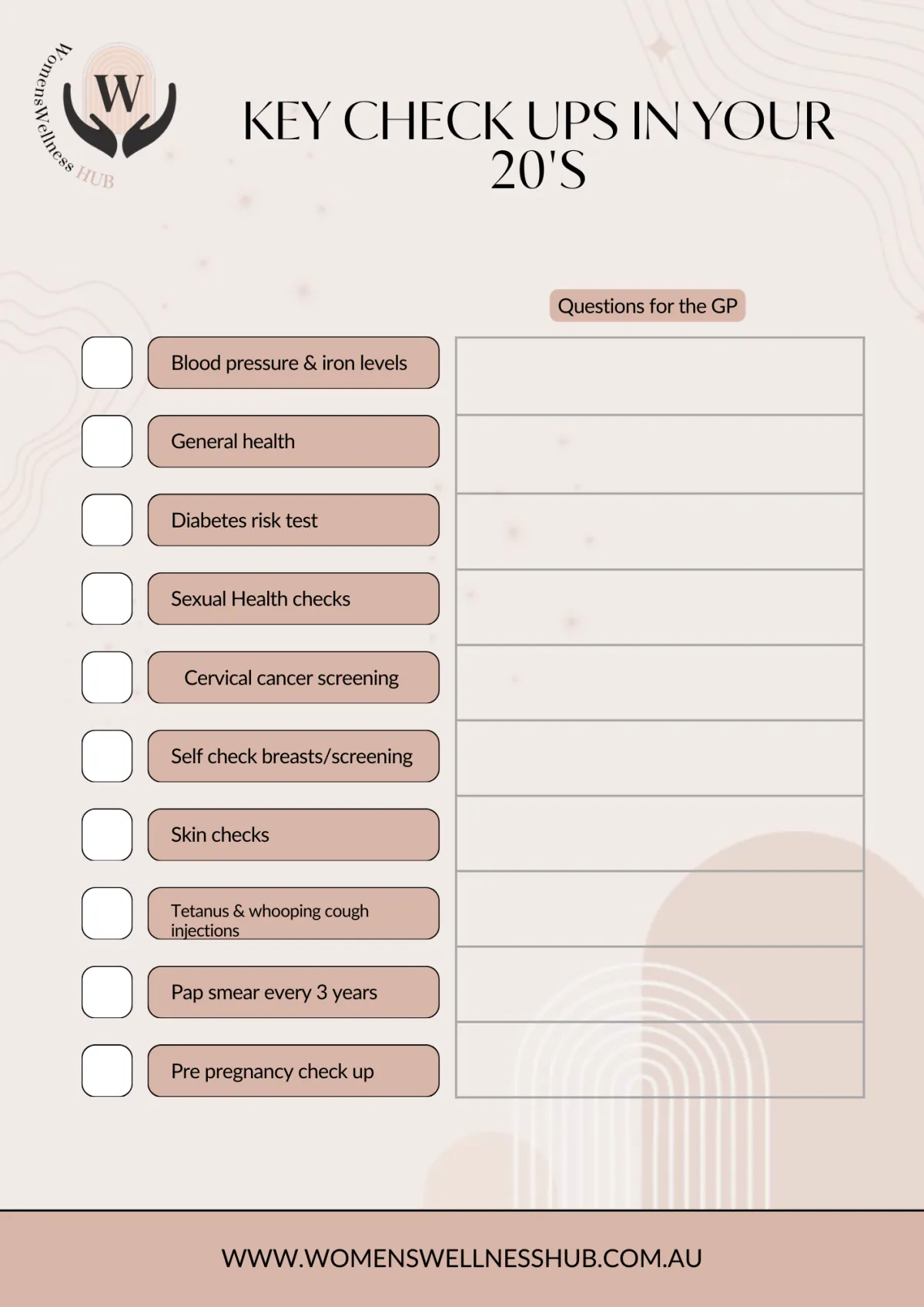
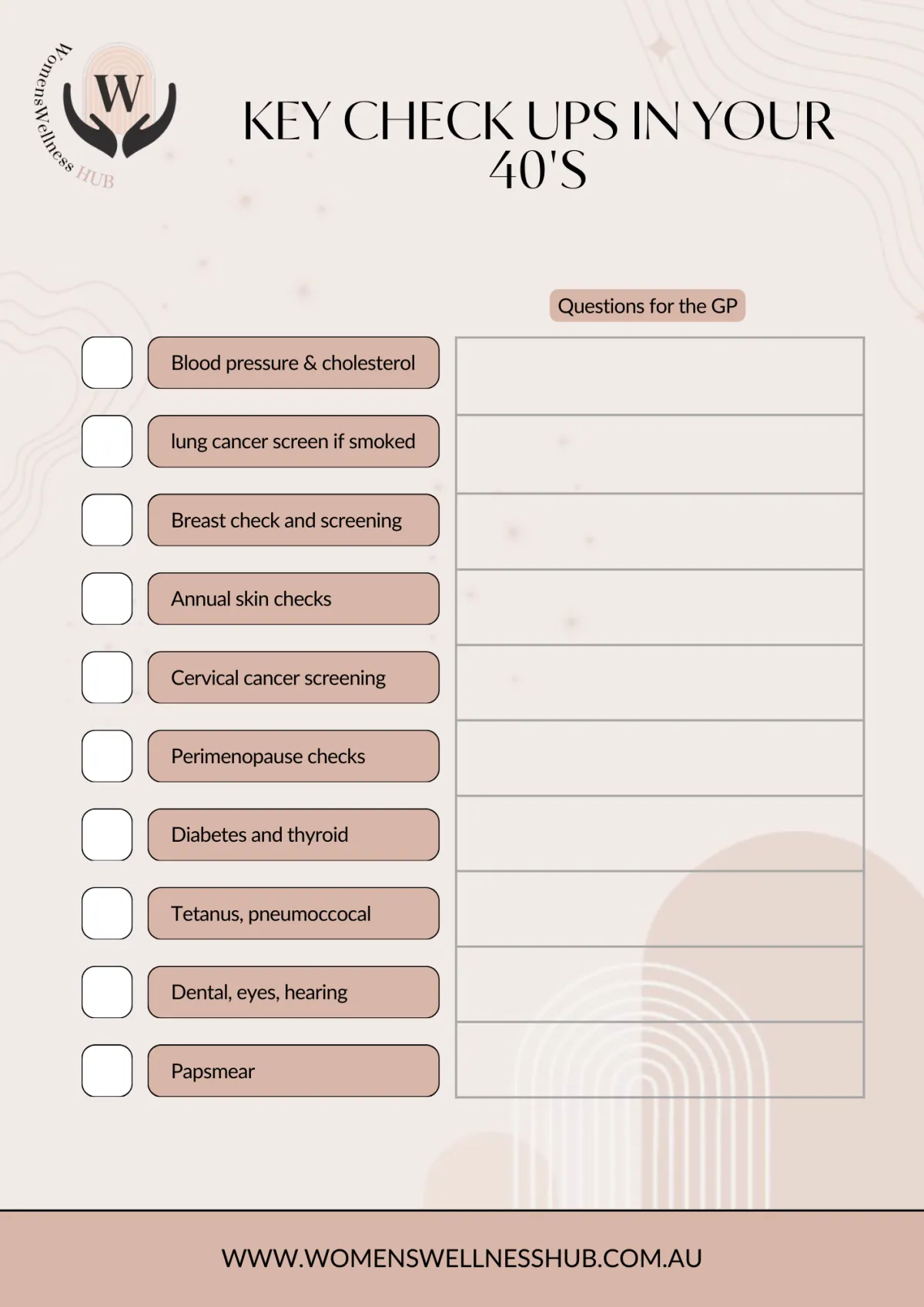
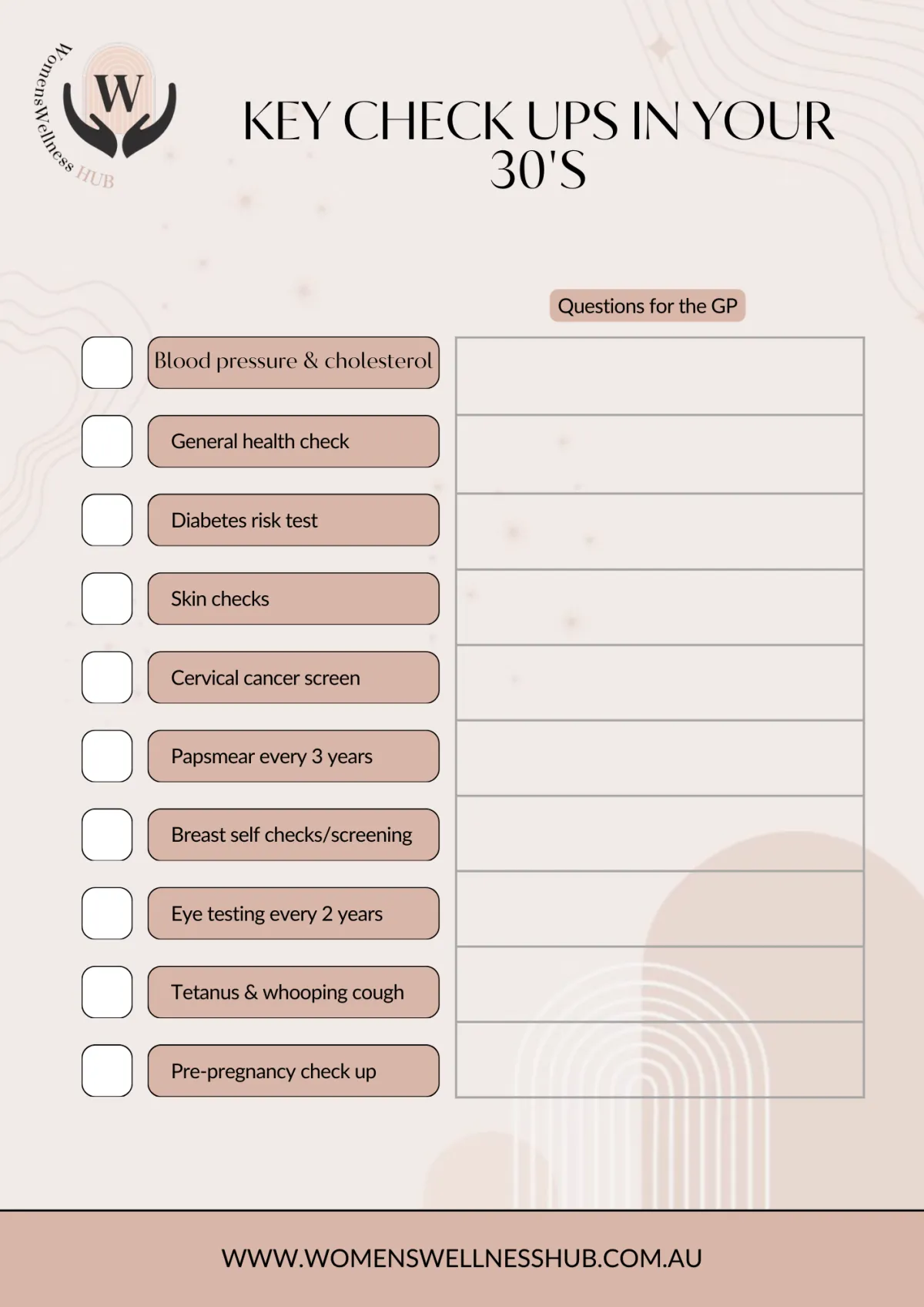
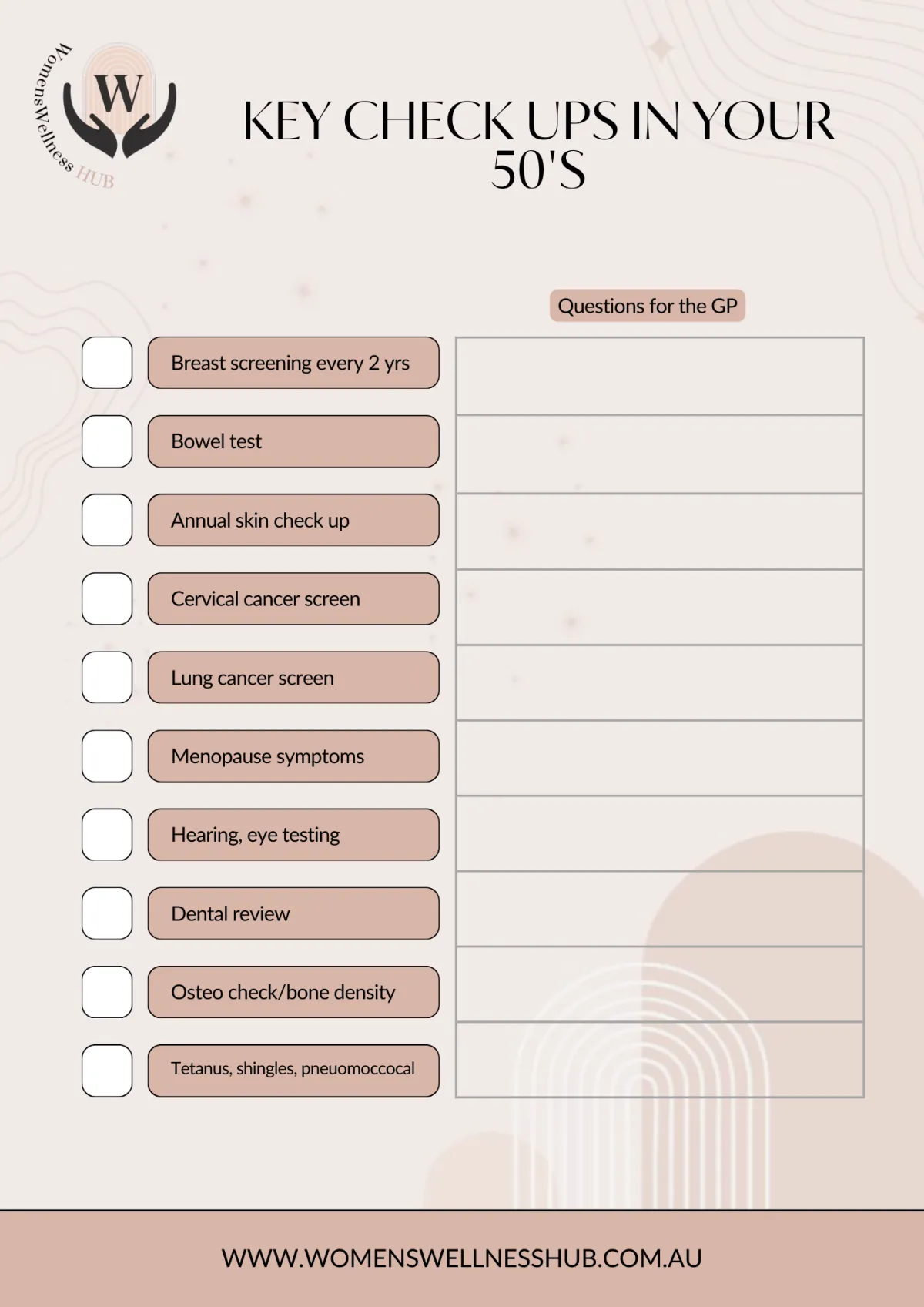
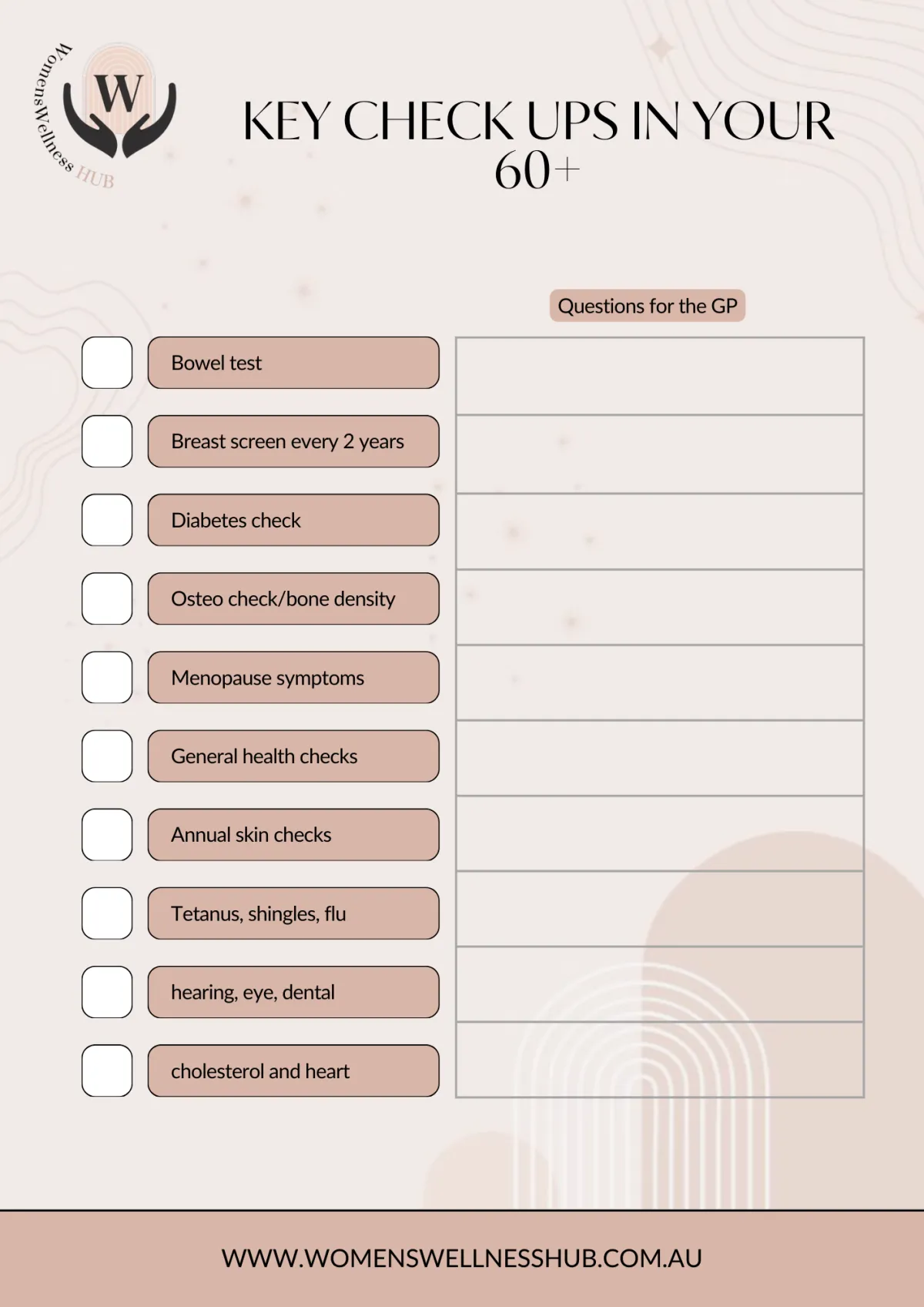
Below are just the key checklists that are medically recommended per decade of a woman's life. Within that decade though you may be required to have the specific checkup or action once (such as tetanus injection usually every ten years) or it may be that in that decade you need to annually do the test with your doctors. For some people who have a family history, prior medical condition, smoke, have other addictions, or just concerns they have noted, the tests in that decade of your life may be significantly more in a bid to try detecting and preventing any heath concerns as soon as possible.
You can interact with this PDF document to add any comments you have in relation to some of these key items.
Why Regular Routine Checks could save your life - even if you aren't feeling unwell
It is a good idea to visit a doctor regularly, even if you feel healthy...... just like your car gets a service, after a certain number of kilometres, even if it seems ok with no obvious sign of repairs.The purpose of these visits is to:
❤️ Check for current or emerging medical problems
❤️ Assess your risk of future medical issues
❤️ Prompt you to maintain a healthy lifestyle
❤️ Update key vaccinations (including but not limited to shingles, tetanus, whooping cough, flu, travel required vaccinations)Health checks are usually incorporated into routine medical care but you may need to ensure you have booked enough time for a review and diarise these checks yourself as you may/may not ever be sent prompts to do it.Having a health check is also a time to examine your lifestyle to see what improvements can be made. This may be something you regularly do yourself or discuss with a healthcare professional.Lorem ipsum dolor sit amet, consectetur adipisicing elit. Autem dolore, alias, numquam enim ab voluptate id quam harum ducimus cupiditate similique quisquam et deserunt, recusandae.

Regular Self Health Checks you can do at Home
You can do a basic health check at home to review your health in relation to:
⛔️ Alcohol consumption - people who have at least 2 alcohol-free days per week and keep their drinking days to 2 standard drinks per drinking day have better long-term health. For more information on alcohol intake and getting additional support refer to this website.
⛔️ Smoking – smoking increases your risk of many diseases, including heart disease, stroke, lung disease and thin bones. If you smoke, quitting as soon as possible helps reduce the harm. For more information on the risks of smoking and how to get help to stop for good, refer to our website.
⛔️ Dental care – cleaning your teeth regularly and eating a low-sugar diet can reduce your risk of tooth loss, tooth decay, gum disease. You should have an annual dental check and professional clean to help reduce these issues. Poor dental health is also often connected to heart disease.
⛔️ Diet and nutrition – a healthy diet improves your general health and wellbeing.For further details on nutrition refer to this website.
⛔️ Physical activity – regular physical activity is good for your mental health, heart and bones, and can prevent many diseases. Ideally the health goal is for 30 minutes to an hour of moderate physical activity a day. Moderate physical activity takes some effort, but it is considered to be at a point where you can still have a conversation (for example, brisk walking, social tennis). Weight training helps considerably, especially in your 40s plus. For more information on stimple exercise strategies for you to follow easily from home or externally refer to our webisite.
⛔️ Routine General Skin checks –currently, there is no set guideline regarding how often Australian adults should get their skin checked. Cancer Council recommends that you regularly monitor your own skin via self-examination and visit a GP if you notice any changes or new suspicious spots (moles, freckles, dark stain/patch etc). A GP can refer you to a specialist if required.However, if you have sunbaked a lot or work outdoors or have a family history of melanoma or other skin disease, you should have a thorough yearly examination by a doctor who specialises in skin checks and/or a dermatologist (get a referral from your GP). A full skin examination, supported with photography and dermoscopy, may be necessary every 6-12 months.While protection from UV radiation is the best defense against skin cancer, regular skin checks via self-examination for new and changed spots and early detection strategies are an important approach to reducing your risk of skin cancer. This is because most melanomas are found by the person with the melanoma, or their partner. For details of how to check for skin cancer refer to the diagram below from Cancer Council NSW.
⛔️ Weight - maintaining a healthy weight range helps prevent longer-term diseases, such as heart disease, diabetes and arthritis. Regular health checks can help to identify early warning signs of disease or illness. Heart disease, diabetes and some cancers can often be picked up in their early stages, when treatment may be more successful.
Routine Breast Checks

Summary of Key Health Checks your Doctor is likely to recommend
When you have a medical check, your doctor will usually talk to you about:
➡️ Your medical history
➡️ Employment (to determine possible impact on your health)
➡️ Your family’s history of disease such a heart, diabetes, stroke.
➡️ Lifestyle generally (including your diet, weight, how much you exercise)
➡️ Whether or not you smoke and drink alcohol or take illegal drugs
Regular health checks may help your doctor pick up early warning signs.
If you have a family history or high risk for other reasons of a particular health condition, your doctor may recommend more frequent health checks at an earlier age.
1. HEART HEALTH CHECKS
➡️ Blood pressure - Your blood pressure is usually checked every 2 years if it is normal, you are aged under 40 years, and there is no family history of high blood pressure.Have it checked yearly or more regularly if you are over 40, your blood pressure is on the high side, or you have a personal or family history of high blood pressure, stroke or heart attack. Be advised by your doctor.
➡️ Blood tests - They will check your cholesterol levels and blood triglycerides, iron levels, and thyroid among other things. High levels may indicate an increased risk of various health problems, including heart disease.If you are over 45, the doctor is likely to suggest blood tests about once every 5 years. If you are at high risk of heart disease and have a family history, you should be tested every year from the age of 40.
➡️ Electrocardiogram (ECG)– this is a non-invasive and painless medical test that detects cardiac (heart) abnormalities by measuring the electrical activity generated by the heart as it contracts.
➡️ Obesity tests – being overweight is a significant risk factor for many health conditions, including cardiovascular disease and diabetes. Ask your doctor to check your body mass index (BMI)and waist measurement every 2 years. If you are at a higher risk, you should have your weight checked more frequently.
Anyone 45 years and over, or 30 years and over for Aboriginal and Torres Strait Islander peoples, should have a regular heart health check with their doctor.
A heart health check is a 20-minute check-up with your GP to assess your risk of having a heart attack or stroke. Heart health checks are covered by Medicare and are free at practices that bulk bill this service.
2. DIABETES TESTS
Diabetes is a serious condition where glucose (sugar) in the blood becomes higher than normal. People with diabetes can have difficulty changing glucose into energy which leads to higher levels of sugar in the blood (hyperglycaemia). Your blood glucose levels are normally controlled by a hormone called insulin.
Diabetes happens when your pancreas can’t produce enough insulin or when your body can’t use the insulin because it’s resistant to it.
Stats in Australia 2024
1,500,000 - People living with diabetes in Australia.
120,000 - People diagnosed with diabetes each year.
400,000- Australians at high risk of diabetesThere are several types of diabetes:
Types of Diabetes
🚩 Type 1 diabetes
🚩 Type 2 diabetes
🚩 Gestational diabetes, which happens when a woman has high blood glucose levels duringpregnancy pre-diabetes, where your blood glucose levels are higher than normal, but not high enough for a diagnosis of diabetes.
What are the most common symptoms of diabetes?
🚩 Being very thirsty or hungry
🚩 Passing more urine (wee) than usual
🚩 Feeling tired
🚩 Unexplained weight loss (for type 1 diabetes), or gradual weight gain (for type 2 diabetes)having cuts that heal slowly
🚩 Itchy skin or skin infections
🚩 Blurred vision
https://www.healthdirect.gov.au/symptom-checker
TYPE 1 diabetes is usually spotted quickly as symptoms can appear suddenly. Many people with type 2 diabetes don’t have any symptoms at all or have signs that go unnoticed for a long time.
TESTING FOR DIABETES
diabetes include a laboratory blood glucose test ordered by your doctor (not using a home blood glucose meter). The most common test is the fasting blood glucose test (no food or fluid except water for eight hours before). Others include a test taken anytime during the day with no preparation, glycosylated haemoglobin (HbA1c) test, or an Oral Glucose Tolerance Test (OGTT).
Talk to your doctor about having your risk of diabetes assessed and how often you should be tested.
AUSDRISK...
You can complete AUSDRISK by yourself, or with the help of a health professional or practice nurse to assess the risk of a person developing type 2 diabetes over the next 5 years.
You can complete the tool in 1 of 3 ways:
➡️ Using the online interactive version
➡️ Using the online non-interactive version
➡️ Downloading the PDF version-and completing it on paper.If you get a 'high' score on AUSDRISK, you are eligible to attend a type 2 diabetes risk evaluation by your GP if you are aged:40 to 49 years (inclusive)15 to 54 years (inclusive) for Aboriginal and Torres Strait Islander people.https://www.health.gov.au/resources/apps-and-tools/the-australian-type-2-diabetes-risk-assessment-tool-ausdrisk
Risk Factors for Getting Diabetes
The exact genetic causes of type 2 diabetes are not currently known however, there is a range of factors that increase the risk of developing the condition.Some diabetes risk factors can be managed or reduced (known as modifiable lifestyle factors), while other factors cannot be changed.
Type 2 diabetes risk factors including - you have pre-diabetes, a family history of diabetes (for example, if you have a first-degree relative with type 2 diabetes) and/or are over 55 years. The risk increases with age, are over 45 years and overweight and obese or have high blood pressure are over 35 years and from an Aboriginal or Torres Strait Islander background, or from a Pacific Island, Indian subcontinent or Chinese cultural background, had gestational diabetes during a pregnancy, have polycystic ovarian syndrome (PCOS)have cardiovascular disease such as past history of heart attack, angina, stroke or narrowed blood vessels taking certain antipsychotic medication or corticosteroid medication.
Other lifestyle risk factors include:
➡️ Being overweight or obese, especially around the waist
➡️ Sedentary lifestyle – having low levels of physical activity, including more than two hours of television watching per day
➡️ Unhealthy eating habits, such as regularly choosing
➡️ High-fat,high-sugar,high-salt or low-fibre foods
➡️ Cigarette smoking.
Maintaining a healthy weightBeing overweight, especially around your waistline, increases your risk of developing type 2 diabetes and losing weight is one way you can help prevent type 2 diabetes. Carrying extra weight around your middle means fat can build up around organs and cause insulin resistance, which means the insulin your body produces doesn’t work properly.A small weight loss (5-10% of body weight) can make a big difference and for those with pre-diabetes can prevent type 2 diabetes in up to nearly 6 out of 10 people. Measuring your waist is a quick and simple way of checking your risk. Measure halfway between the top of your hip bone and your lowest rib, roughly in line with your belly button.
According to Diabetes Australia, the general rule of thumb is, if you are of Caucasian origin:
Women should aim for a waist circumference less than 80 cm
Men should aim for less than 94 cm
There are no quick fixes when it comes to reducing your waist size but small changes in your diet (such as reducing your portion size) and regular physical activity are important factors in weight loss and maintaining a healthy weight. Advice from a dietitian, exercise specialist or other health care professionals can make losing weight much easier and sustainable.Making healthy food choicesEating a healthy, balanced diet is way great way to manage your weight and reduce your risk of developing type 2 diabetes.
As a starting point, Diabetes Australia recommend people follow the Australian Dietary Guidelines. https://www.eatforhealth.gov.au/guidelines/guidelinesRegular physical activity to reduce diabetes risk factorsRegular physical activity is key to preventing type 2 diabetes as it helps to maintain a healthy weightlower your blood pressure and reduce your risk of heart disease and stress.T
The Australian Government’s physical activity and exercise guidelines for all Australians recommend adults should be active most days, preferably every day. Moving for at least 30 minutes a day makes a big difference to your health and wellbeing. It also helps lift your mood. You can break up exercise throughout the day if needed.You don’t need to go to the gym or run a marathon, aim for moderate intensity. It could be a brisk walk around your suburb, playing a sport in the garden, or doing an online exercise class.
More information
Check your risk
Find out your risk of developing type 2 diabetes within the next five years. Check out the risk calculator on Diabetes Australia
Introducing Diabetes YOUnited – our new national membership program. We want all Australians, no matter where they live or their financial situation, to have access to essential support.
3. BOWEL CANCER CHECKS
Bowel cancer is one of the most common cancers in Australia.The National Bowel Cancer Screening Program reduces illness and death from bowel cancer by detecting the early signs of the disease using a free, simple test that can be done at home.
Bowel cancer often develops without any symptoms. The cancer can grow in the bowel for years before spreading to other parts of the body. Very small amounts of blood can leak from these growths and pass into your faeces (poo). These tiny amounts of blood are not noticeable just by looking – that's where screening comes in.Screening can find tiny amounts of blood in your poo that may be a sign of bowel cancer. The good news is that if found early, over 90% of bowel cancers can be successfully treated.
Screening for bowel cancer in people aged 45 to 74 who do not have any symptoms, helps to find cancer early. The bowel cancer screening test uses chemicals to check a bowel motion sample for blood, which may be a sign of bowel cancer.
Eligible Australians aged 45 to 74 can do a free test at home every 2 years. Learn about the program and how to do the test on https://www.health.gov.au/our-work/national-bowel-cancer-screening-program
The National Bowel Cancer Screening Program sends free test kits in the mail to people aged 50 to 74, every 2 years (to the address connected to your medicare card). If you are between the age of 45-49, you can also request your first free bowel screening kit to be mailed to you. If you have a family history of bowel cancer, please talk to your doctor about what screening options are right for you. People at high risk of bowel cancer may need a colonscopy more regularly. During this test, the doctor inserts a slender instrument called a colonoscope through the anus to visually check the rectum and large bowel for any abnormalities.
You may receive reminders to complete the test via SMS if we have your mobile number. If you would prefer to get reminders in the post, follow the instructions in the SMS or update your communication preferences in the National Cancer Screening Register (NCSR) Participant Portal.
The bowel screening test is an immunochemical faecal occult blood test (iFOBT). It can detect tiny amounts of blood in your poo that can be a sign of bowel cancer.You just need to collect 2 tiny samples from 2 different poos. Then mail them to the pathology lab in the reply paid envelope with the completed participant details form.
You can watch a video on how to do the test at www.health.gov.au/national-bowel-cancer-screening-program. You and your doctor receive the results within 4 weeks.
4. EYE CHECKS FOR VISION AND EYE HEALTH
Eyesight tends to deteriorate with age. Serious eye concerns can include cataracts, skin cancer on the eye, cataracts, mascular degeneration,diabetic retinopathy.People older than 65 years should have an annual examination, however, more frequent testing may be recommended for those with certain risk factors, such as:➡️ a family history of eye disease,➡️ a personal history of eye disease or injury,➡️ certain medical conditions such as high blood pressure or diabetes, taking certain medications.If you already wear prescription glasses or contact lenses, you should have your eyes tested every year. Adults who do not wear prescription glasses or contact lenses should have an eye test every 2 years.
In Australia, regular eye tests by an optometrist are crucial for early detection of eye problems and maintaining good vision, and are often bulk-billed for eligible Medicare card holders. Here's a more detailed explanation:Importance of Eye Tests:Regular eye tests are vital for detecting eye diseases early, which can help prevent vision loss. What to Expect:During an eye test, an optometrist will check your vision at various distances, assess eye health, and potentially test for conditions like glaucoma or cataracts.
Types of Tests:
Common tests include visual acuity tests, tonometry (measuring eye pressure), slit lamp exams (examining the eye's structures), and refractive tests (determining the need for glasses or contact lenses). Frequency:Most people should have an eye test every two to three years, or more frequently if recommended by your optometrist. Medicare Coverage:Eye tests are often bulk-billed for eligible Medicare card holders, meaning there's no out-of-pocket cost. Finding an Optometrist:You can book an eye test online or by calling optometrists like Oscar Wylee, Specsavers, or OPSM. Online Eye Tests:Some websites offer online eye tests, but these are not a substitute for a comprehensive eye examination with an optometrist. Eyesight Tests for Drivers:If you are renewing your driver's license online, Transport for NSW may defer your eyesight test if you are a low-risk driver.
Medicare Payments
Medicare will pay for your eye test if the optometrist chooses to bulk bill. If you're under 65, you can have one bulk billed eye test every 3 years. If you're over 65 you can get a bulk billed test yearly.

These are some common tests, but your doctor may recommend others according to your situation.
SUMMARY OF HEALTH CHECKS OFTEN SUGGESTED BY YOUR DOCTOR:
Your Title Here
Lorem ipsum dolor sit amet, consectetur adipisicing elit. Autem dolore, alias, numquam enim ab voluptate id quam harum ducimus cupiditate similique quisquam et deserunt, recusandae.

Your Title Here
Lorem ipsum dolor sit amet, consectetur adipisicing elit. Autem dolore, alias, numquam enim ab voluptate id quam harum ducimus cupiditate similique quisquam et deserunt, recusandae.

Your Title Here
Lorem ipsum dolor sit amet, consectetur adipisicing elit. Autem dolore, alias, numquam enim ab voluptate id quam harum ducimus cupiditate similique quisquam et deserunt, recusandae.

5. STI'S Sexually transmissible infections (STI) screening
If you are sexually active, you should get tested for chlamydia every year between the ages of 15 and 29, using a simple urine test. Chlamydia is very
common and does not always show symptoms.
If you are at risk of other sexually transmissible infections such a herpes or HIV/AIDS raise your concerns and ask your doctor about further testing.
6. BONE DENSITY CHECKS - OSTEOPOROSIS
Advancing age is a significant risk factor for osteoporosis. Osteoporosis is a disease characterised by low bone density and the weakening of the building blocks that make up your bones.
People living with osteoporosis have porous, fragile bones, which can lead to an increased risk of fractures (broken bones).
If you have higher-than-average risk factors for osteoporosis your doctor might refer you for a bone density scan.
Bone density scans are widely accessible, painless, are often covered by Medicare and involve minimal levels of radiation.
What is a bone density scan?
A bone density scan is a medical test used to help diagnose osteoporosis and are also used to help see whether your risk of developing osteoporosis in the future is
higher than average. As a result, people living with osteoporosis have porous, fragile bones, leading to an increased risk of bone
A bone density scan is also known as a bone density test, a bone mineral density test or by its medical name, a DXA test.
How does a bone density scan measure my bone strength?
A bone density scan is done using a special type of x-ray called a dual energy x-ray (DXA). The DXA measures bone mineral density. The scan gives you and
your doctors information about your bone strength or fragility (weakness), and your risk of fractures. In general, the lower your bone density, the higher your risk of having broken bones in the future.
Do I need a bone density scan?
If you are at risk of getting osteoporosis, your doctor will refer you for a bone density scan.
People with an average risk of getting osteoporosis include:
➡️ post-menopausal
➡️ females aged 45 years and and males over 50 years
➡️ People with a high risk of osteoporosis include males over the age of 60 years and females over the age of 50 years who also:
➡️ have a family history of a fragility fractures
➡️ smoke or have a high alcohol intake
➡️ have vitamin D deficiency
➡️ have low body weight
➡️ have recurrent falls
➡️ are immobile (cannot walk or do housework without help) or have low levels of physical activity.
Some medical conditions can also put you at an increased risk of developing osteoporosis. If you have one of these conditions, your doctor may refer you for a bone density scan.
Health conditions include:
➡️ endocrine (hormone) disorders
➡️ early menopause
➡️ anorexia nervosa
➡️ inflammatory conditions and conditions causing malabsorption(problems in your digestive tract or gut)
➡️ chronic kidney or liver disease
➡️ diabetes
➡️ HIV
Taking certain medicines can also increase your risk of osteoporosis, so if you take one of the following medicines, your doctor may refer you for a bone density scan to check your bone health.
Your doctor will review all factors and assess your overall fracture risk. If you have already had a fracture, and based on your other risk factors, your doctor will work out if your risk of more fractures is higher than average. If you are, you will most likely be referred for a bone density scan.
For example, if you are over 45 years of age, and have broken a bone after a minor fall or incident (known as a ‘low-trauma fracture’), if you are a female who has gone through menopause or if you are an older male who has had a vertebral fracture (a break to one of the bones in your spine), you will likely need a bone density scan.
7. Breast cancer screening - 1-7 Australian women - are you eligible and been to have your breast screen? BOOK IN! Even if you are not eligible, GO SEE THE DR!
Breast cancer is the most common cancer affecting Australian women. It can occur at any age, but it is more common in women over 60.
Watch the important Utube video - "listen to your body- make the effort to book in and have a scan to look after your body." It's the ultimate act of self care!
Breast screening (also known as mammogram) is one of the best ways to detect breast cancer early. If breast cancer is found early, it is more likely to be successfully treated and improve your chance of surviving it.
BreastScreen Australia invites women aged 50 to 74 for free mammograms every 2 years.
If you are in your 40s or over 75, discuss the risks and benefits of screening with your doctor. Women under 40 are not eligible for the screening program but can have a mammogram done with a GP's referral at any age.
It is important that at any age, if you notice any breast symptoms or a change in the look and feel of your breast to see your doctor without delay.
8. Cervical screening test
Having regular cervical screening tests can help prevent cervical cancers through early detection and treatment.
Cervical cancer screening is recommended every 5 years for women and people with a cervix who are aged 25 to 74 years and have ever been sexually active.
The cervical screening test (which replaced the pap test) checks for the presence of the human papilloma virus – a virus that can cause cervical cancer.
Even if you have been vaccinated against HPV, regular cervical screening is still important as the vaccine does not protect against all types of HPV infection.
Screening is available for eligible people through the National Cervical Screening Program.
You can usually collect your own vaginal sample if they choose, this is called self-collection. Self-collection is a safe and effective method of testing.
9. Pregnancy
You should have a general check-up before becoming pregnant to discuss any health risks during pregnancy. Once you are pregnant, regular antenatal checks help monitor your baby’s development, pick up abnormalities and assess your health.
Tests related to pregnancy may include ultrasound scans, urine tests, blood tests and genetic testing.
Some antenatal tests are recommended for all pregnant women, while others are only necessary for women at increased risk of complications.
Be advised by your doctor.
You can book an eye test directly with an optometrist. You don’t need a referral from your GP.
If you notice any changes in your vision, you should get an eye test. If you see your GP about your vision, they may suggest you go to an optometrist.
Use the
find a health service tool
on the healthdirect website to find an optometrist near you.
We will pay for your eye test if the optometrist chooses to bulk bill. If you’re under 65, you can have one bulk billed eye test every 3 years. If you’re over 65 you can get a bulk billed test yearly. Not all optometrists bulk bill. Read more about
bulk billing
.
We don’t cover the cost of glasses or contact lenses. If you have private health insurance it may help pay for these, depending on your level of cover. Read more about
private health insurance and Medicare
.
Most states and territories have programs that help to pay for glasses and contact lenses. Read more about
eye health schemes
on the Department of Health website.
If you have an eye disease or disorder you may get a referral to an ophthalmologist. They are specialist eye doctors who can perform surgery. Before your appointment you should ask about the cost and if they bulk bill.
Getting help with hearing tests
If you notice any changes in your hearing, you should see your GP. They can refer you to an audiologist for a hearing test to measure any hearing loss.
You may be able to get hearing tests through the Hearing Services Program. The program may also cover some or all of the costs of hearing aids. If you’re not eligible for the program, you may get lower cost aids through a hearing aid bank.
Visit the
Hearing Services Program
on the Department of Health and Aged Care website to find out:
how to applyhow to find a hearing aid bank near you.
Getting help with diagnostic imaging and scans
Diagnostic imaging and scans allow doctors to view and take images of the inside of your body. The type of imaging depends on your symptoms and what your doctor needs to see. Your doctor will decide what scans you need and give you a referral. Diagnostic imaging and scans include:
X-raysCT scansnuclear medicine scansMRI scansultrasound.
Most imaging is painless. You just need to stay still for a period of time inside a machine. Some tests involve exposure to some radiation. For some tests you may need an anaesthetic.
Diagnostic imaging providers set their own fees. Before your test you should ask how much you will have to pay. If the provider chooses to bulk bill you, you won’t have to pay. Read more about
bulk billing
.
Your doctor may give you a form for one brand of diagnostic imaging provider. You are free to choose your own provider as long as they offer the scan you need.
You can choose to add your diagnostic imaging reports to your My Health Record. This means you and your doctor can access them. Read more about
My Health Record
on the Australian Digital Health Agency website.
Next:Other Medicare support
We have a range of programs to help with some specific health care needs.
Menopause Support Centre
Your step by step guide to the PAUSE!
We hear you, we understand, we are here to support you.
What to ask at the doctors
Women's Wellness Hub Directory
Thank you to our wonderful sponsors and ambassadors

How I lost my mojo thanks to Perimenopause
How I lost my Mojo at home and work thanks to Perimenopause!
I was 45 years old and suddenly felt like I had been hit be a tidal wave.
I felt burnt out, sleep deprived, self-conscious and unable to perform as well as I used to at work.
I had surges of hot flushes which periodically drenched me, was a lot more irritable and impatient with fellow staff and clients, had a frozen shoulder and aching knee, had some brain fog, especially with peoples names, and general exhaustion. There were days when I just wanted to walk out of the office and never return. I could barely cope at home with the kids and my husband, let alone deal with co-workers.
I can recall being performance managed for my comments in a workplace meeting which in hindsight were too outspoken, but I just seemed to lose the ability to hold back my opinions which I had once reserved.
Ironically, despite knowing quite a lot at the time about menopause, I still considered myself too young, I only had a 7 year old child, still had consistently heavy periods and there was nothing that made me initially think it was perimenopause. I actually thought I had a very, very long winded case of the flu.
As incredible as it seems, with 50% of the population going through it, most women still don’t know the basic facts about perimenopause and menopause, making it difficult to identify hormonal changes as a potential cause for not feeling well. In turn they are often not seeking the support and treatment options which could really provide them with significant symptomatic relief.
Our mothers were often also uneducated on the topic and/or quiet about it, there was no education at school and most of the medical fraternity have been poorly educated themselves about how to identify, treat and support. My own doctor wrote it off as anxiety caused by life challenges at the time, and prescribed me anti-depressants and melatonin for sleep.
Like me, many of my menopausal workmates, have felt neglected, overlooked, embarrassed and frustrated and opted to simply leave work, retire early, reduce their work hours, not apply for promotional opportunities, merely because they were feeling overwhelmed and insecure as a result of their physical and psychological menopausal symptoms.
As recently highlighted by the Senate inquiry into Menopause, workplaces need to better accommodate women who experience symptoms of menopause and perimenopause.
“All employers have a responsibility to address stigma around menopause in their workplaces. Implementing organisation wide menopause policies, promoting internal awareness for employees and managers about these issues and sharing menopause-specific workplace resources can all help to address menopause stigma.”
We are often in the prime of our careers when perimenopause symptoms strike, with an enormous amount to still offer an organisation. It is an inevitable time in our lives but it can be challenging and we need workplace support to help us get access to information about the symptoms, treatment options and lifestyle changes we may need to continue to be as productive, confident and empowered.
Better psychosocial risk assessments which include support for menopausal employees, menopause awareness training at work, workplace policies and procedures, flexible working arrangements are all steps in the right direction but it is still uncommon to find this level of support in many organisations.
At Corporate Wellness Solutions we look deeper at what amounts to a psychosocial hazard rather than just what the Code guides us on. That is why I decided to add menopause to our psychosocial wellness solutions programs.
We can provide you with all the perimenopause and menopause information and education from the experts, policy templates, conversation guides and prompts to initiate menopause conversations with managers and employees (from both perspectives), symptom trackers, checklist for businesses to compare how menopause friendly their workplace is and a wellness support program tailored to your employee needs.
This site is brought to you by Family Counselling Support Network
Book in directly with one of our professionals today

We are here to help

We are committed to protecting your personal information and respecting your privacy. This website uses cookies to analyze website traffic and optimise your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.
DISCLAIMER: The material contained on this website is for general educational and information purposes only and is not a substitute for professional legal, financial, medical or psychological advice or care. While every care has been taken in the information provided, no legal responsibility or liability is accepted, warranted or implied by the authors or Family Counselling Support Network and any liability is hereby expressly disclaimed. For specific advice please contact us at [email protected]. All information contained on the website remains the intellectual property of Family Counselling Support Network and is for your personal educational use only. The information must not be reproduced or distributed without the express permission of Family Counselling Support Network.
Family Counselling Support Network acknowledges and respects the First Nations Custodians of the land where our offices stand, and where we work to help Australians. We pay respects to their Elders, past present and emerging, lore, customs and creation spirits. We recognise that these lands have always been places of ceremony, teaching, research and learning, and we acknowledge the important role Aboriginal and Torres Strait Islander peoples play in our community.
We are committed to providing an inclusive and accessible environment where people and communities of all identities and backgrounds are accepted, safe and celebrated.
Privacy Policy | Terms and Conditions